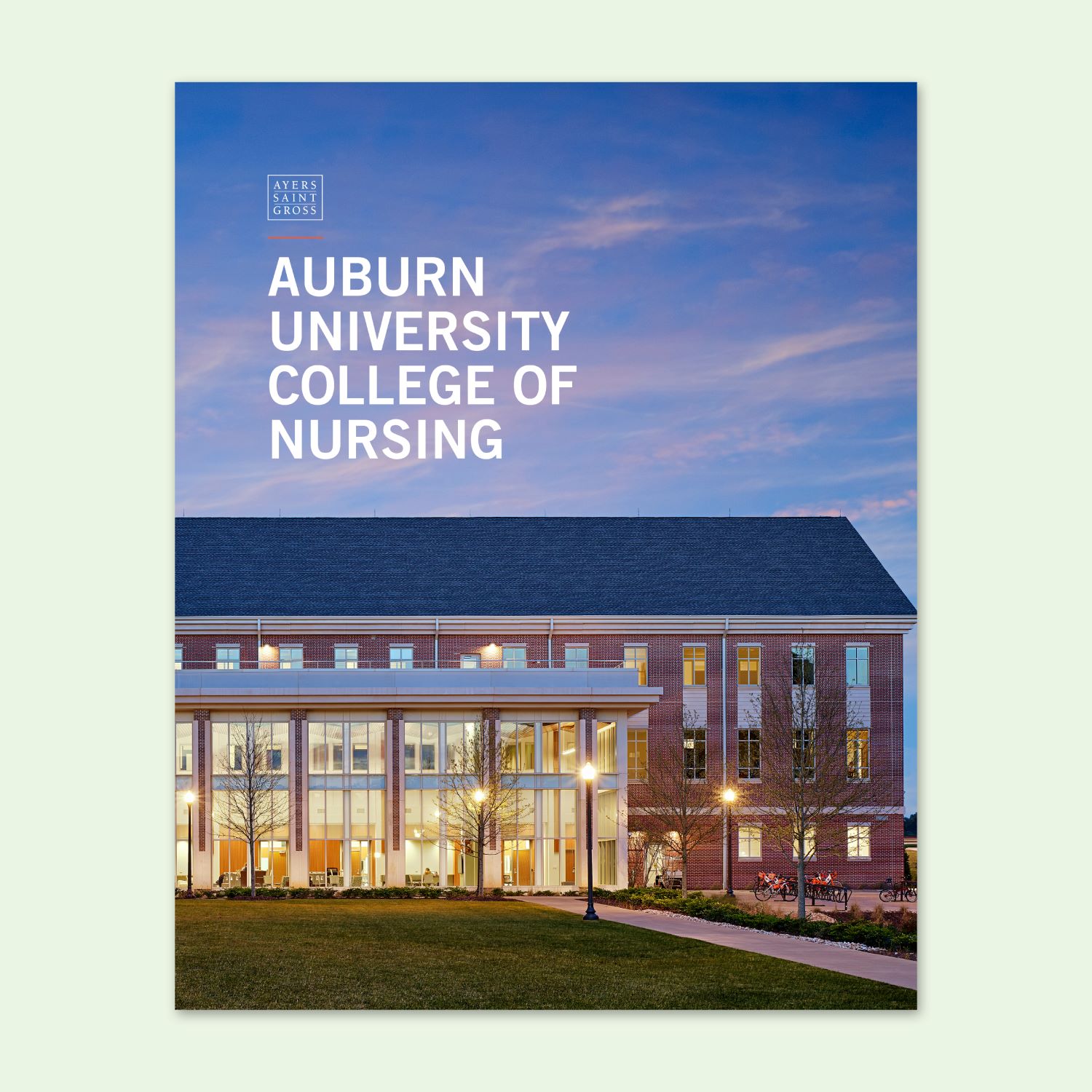
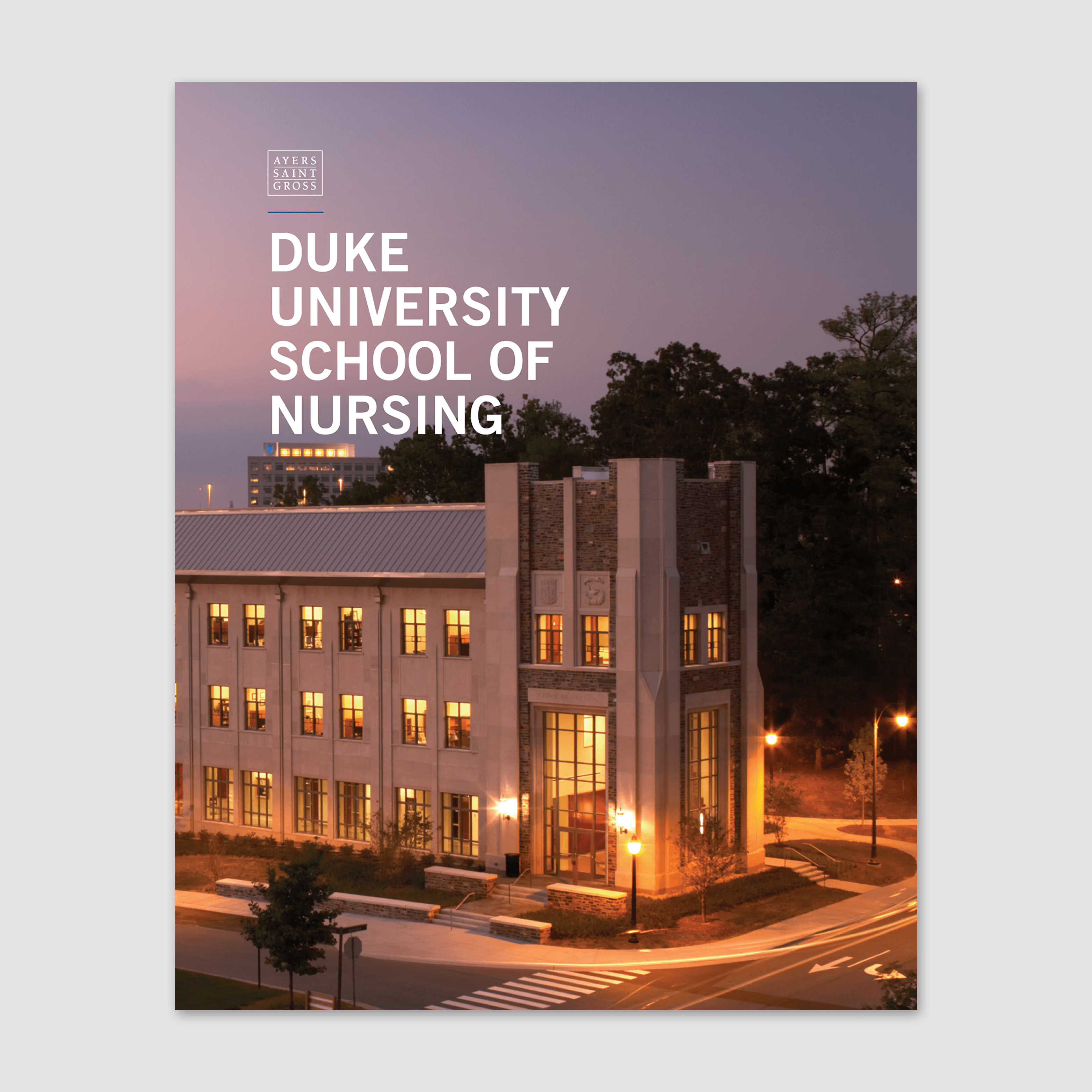
As leaders in nursing school design, Ayers Saint Gross has closely followed the evolution of nursing education in recent years. Schools are adapting to overcome challenges related to the nursing shortage, COVID-19, remote learning, and more. Ayers Saint Gross works alongside many institutions as trusted advisors to plan and design best-in-class spaces to support the future leaders in nursing.
Simulation-based education has increased over the past few decades and continues its widespread implementation throughout all levels of nursing education; it is the gold standard for educating modern nurses and healthcare professionals.